BACKGROUND: In 2019, the Hematology/Oncology Pharmacy Association (HOPA) and the Academy of Managed Care Pharmacy (AMCP) convened a forum to discuss the use of value-based care models in oncology, emphasize the importance of pharmacist involvement in implementing value-based care at their institutions, and create a white paper on this topic.
OBJECTIVE: To highlight areas of opportunities for oncology pharmacists to participate in the implementation and delivery of value-based care in oncology.
DISCUSSION: This white paper summarizes the HOPA/AMCP forum and serves as a call to action to health system pharmacists to engage in the continuum of cancer care as essential providers of value through the implementation of quality processes that inform safe and effective treatment choices, enhance patient satisfaction with care, and reduce unnecessary healthcare costs. Panel discussions provided examples of successful collaborations between health systems and payers, enabling data exchange and risk stratification of patients and subsequent reorganization of pharmacy resources from volume to value-based activities.
CONCLUSION: The forum’s recommendations urge pharmacists to engage in the practice of value-based oncology care and will be shared with patient groups, providers, and policymakers to move this conversation forward.
J Hematol Oncol Pharm.
2020;10(4):212-219
The rising costs of cancer care and the aging US population pressure healthcare systems to deliver high-value care while managing costs. Chemotherapy drug prices continue to increase with advances in precision medicine and immunotherapy, with Medicare bearing the larger burden of costs. A 2013 Institute of Medicine (IOM) report on the state of cancer care showed that costs of cancer care are the highest among other healthcare expenditures and are expected to reach $173 billion to $207 billion in 2020.1 Moreover, the cost of treating cancer poses a significant financial burden on patients, negatively affecting their quality of life (QOL).1,2 In addition, the IOM report showed that cancer care was often neither patient-centered nor demonstrative of quality.1
In 2015, the Centers for Medicare & Medicaid Services (CMS) passed the Medicare Access and Children’s Health Insurance Program (CHIP) Reauthorization Act (MACRA) to incentivize practices to focus on the delivery of quality care while managing costs.3 Through the Quality Payment Program (QPP), Medicare payments are now linked to performance on quality programs and metrics.3 Within health systems, pharmacists are central to cancer care and have opportunities to partner with clinicians at every level of care to improve outcomes. Pharmacists’ involvement in value-based care has been documented in the primary care model.4-13
On June 18, 2019, the Hematology/Oncology Pharmacy Association (HOPA) and the Academy of Managed Care Pharmacy (AMCP) convened the forum “Value of Cancer Care: Pharmacy Call to Action” in Washington, DC. The goals of the forum were to (1) summarize key points on the use of value-based care models in oncology; (2) emphasize opportunities for and the importance of pharmacist involvement in implementing value-based care at their institutions/practice sites; and (3) create a white paper that emphasizes areas of opportunities for oncology pharmacists in value-based care.
A premeeting survey of forum attendees showed gaps in knowledge about value-based frameworks and their application in practice, and a desire to receive education about value-based payments. Survey responders identified several barriers to the delivery of value-based care, naming lack of personnel, lack of funding, infrastructure challenges, and inefficiencies. The forum gathered health system pharmacists, regional healthcare leaders, pharmacy benefit managers, and employers to engage in a discussion regarding pharmacist involvement in value-based care.
This white paper reviews value-based care models and frameworks and highlights opportunities for pharmacists to participate in quality programs, actively engage in enhancing value for patients and clinicians, and reduce the cost of care. It also serves as a pharmacy call to action for pharmacists in their respective practices.
Opportunities for Health System Pharmacists
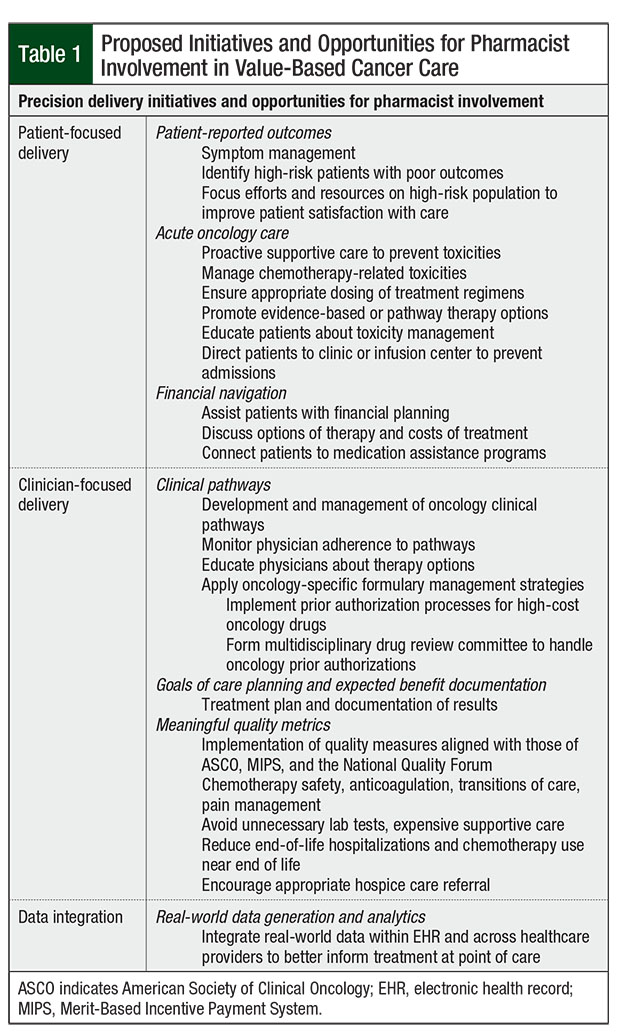
Within hospital systems, the 3 pillars of value-based cancer care focus on patients, providers, and data. Patient-focused delivery, the first pillar, consists of collecting patient-reported outcomes (PROs), offering acute oncology care, and assisting with financial navigation. Clinician-focused interventions include the development of clinical pathways, defining the goals of care, treatment planning, and implementation of quality metrics endorsed by national quality organizations. Finally, meaningful use of data within enhanced electronic health record (EHR) systems will lead to a better assessment of value.
Patient-directed opportunities include tracking and monitoring PROs with electronic alerts through patient self-reporting of symptoms, such as those often associated with anticancer therapy. According to Basch and colleagues, monitoring PROs was associated with early responsiveness and prevention of adverse events, fewer emergency department visits and hospitalizations, and ability to tolerate continuation of chemotherapy longer compared with standard symptom reporting.14
In addition, an overall survival benefit was noted by Basch and colleagues in an earlier study among patients who self-report outcomes.4 Collection of PROs generated more clinical interventions by healthcare personnel, including outreach calls for symptom management counseling, supportive medications, chemotherapy dosage modifications, and referrals to care.4 Collecting PROs for even select populations of patients, such as high-risk patients, may be valuable in identifying those who may be more likely to have poor outcomes. Earlier interventions for this patient group may improve outcomes and increase patient satisfaction with care.
Pharmacist-based optimization of acute oncology care is yet another value-added service that can benefit patient-focused and clinician-focused care delivery. Pharmacists can work with providers to help select the best treatment plan for each patient and ensure that drugs within the plan are appropriately dosed and supportive care is provided. Meeting with patients to provide education regarding their treatment, monitoring plan, and management of potential adverse effects is an important part of the overall treatment plan and can minimize complications for patients when they are sent home.
According to Panattoni and colleagues, on average, patients receiving chemotherapy visit the emergency department twice annually.6 In their study, they concluded that the prevalence of potentially preventable cancer-related emergency department visits could be substantial (41%-63%). Furthermore, overutilization of the emergency department resulted in increased hospital admissions and healthcare costs.6 Reducing unnecessary emergency department use in oncology has been a focus of Medicare quality improvement programs and is tied to reimbursement.
The Oncology Care Model (OCM) now incorporates quality indicators, such as unnecessary hospital admissions, readmissions or emergency department visits, and treatment-related emergency department visits. Hunis and colleagues created an organizational protocol to decrease emergency department visit rates through identification of the causes of admissions, intervention recommendations, and outcome measurements.7 Implementation of a telephone triage protocol to identify emergent symptoms and chemotherapy adverse events resulted in a 60% decrease in the number of patients visiting the emergency department through positive interventions. In this model, protocols were developed to help the triage staff handle patient calls.7 Pharmacists’ expertise can be valuable for developing such protocols and supporting the triage personnel.
Attendees at the HOPA/AMCP forum advocated for the important role of pharmacists in assisting physicians and patients with financial navigation of managing patients with cancer. Financial difficulties that patients with cancer encounter as drug costs rise (now known as financial toxicity) were associated with psychological distress, delayed access to subsequent care, nonadherence to treatment, and a negative impact on treatment outcomes.2 According to a recent analysis, average healthcare spending for patients with cancer reaches $25,000 in the month of diagnosis, and high out-of-pocket costs persist well after diagnosis.15 Thus, integrating cost discussions between physicians and patients is critical to delivering quality cancer care.16
Pharmacists and other members of the pharmacy department can serve as a resource for drug financial assistance programs, advising providers and patients. The use of medication assistance programs may lessen the financial burden on patients as well as on the healthcare system.
Additional clinician-focused initiatives center on clinical pathways and meaningful quality metrics. A retrospective multicenter cohort study evaluating the implementation of clinical pathway programs demonstrated a 35% reduction in patient costs among adhering physician practices compared with other practices.17 Pathways reduce variability in healthcare delivery, which is a well-recognized source of increased costs.18 Insurance companies are progressively integrating clinical pathways developed by private companies, and using them to assist in formulary inclusion and coverage decisions, as well as to inform appropriate treatment and supportive care options for oncologists.17
Pharmacist skills are required to develop and update pathways, as well as to establish a schedule for pathway formulary reviews as new data for existing and novel therapies emerge and guideline updates are published. Pharmacists monitor and audit physician utilization and adherence to pathways and evaluate clinical data for the utilization of off-pathway drugs in special populations. In addition, pharmacists may propose oncology-specific formulary management strategies to assist with coverage decisions and drive the use of cost-effective drug therapies. For example, requests for prior authorization can be submitted to a multidisciplinary team that includes physicians, pharmacists, social workers, nurses, and allied healthcare professionals.
Pharmacist-led initiatives can address practice-based oncology quality measures. Examples include initiatives that focus on the patient-reported experience and satisfaction with care. In addition, treatment planning, chemotherapy handling and administration, patient adherence to treatment, toxicity or complication management, and patient education are all examples of where pharmacists can provide value within their practices.
Finally, a learning health system model that can collect and rapidly analyze real-world data within EHRs is urgently needed to inform answers to clinical questions. Learning health systems generate continuous knowledge at the clinical point of care through linkages and mining of big data sets, collaboration between providers and patients, increased research in practice-based settings, exchange of clinical information in real time, and quality improvement processes.19
In today’s clinical practice, the capabilities of learning health systems remain suboptimal. Pharmacists can fill in gaps in different areas of data analysis, collaboration within the multidisciplinary healthcare team, research, and quality improvement. A summary of pharmacist initiatives to support value-based care is provided in Table 1.
Overview of MACRA Legislation and the Quality Payment Program
The recently introduced MACRA legislation rewards quality and value-based care through the QPP. MACRA promises to deliver high-value, high-quality cancer care while controlling cost and achieving best outcomes at the lowest cost.3 Value-based reimbursement motivates practices to transform the delivery of cancer care through the QPP.
Some objectives of the QPP include improved patient health by improving care; lowering associated healthcare costs; advancing the use of healthcare information between providers and patients; educating and empowering patients; maximizing program participation with easy-to-use tools, education, outreach, and support; and providing actionable performance data to stakeholders with continuous improvement based on feedback and collaboration.
Medicare QPP is delivered via the Merit-Based Incentive Program System (MIPS) or through alternative payment models (APMs).3 MIPS collects physician-reported data related to the program’s quality measures and rewards physician practices based on their performance. MIPS calculates a final score, the “QPP performance adjustment score,” used to adjust the set physician fee schedule. As shown in the Figure, the MIPS score is divided into 4 large categories, including general and oncology-specific quality measures (45%), interoperability or meaningful use of updated EHRs (25%), attestation of improvement activities (15%), and overall cost of care (15%).3
Participation in MIPS is mandatory, unless physicians are exempt, or if they qualify for APMs such as accountable care organizations, capitated model, or integrated care system. In advanced APMs, participating providers may suggest innovative payment mechanisms, new systems for care delivery, or clinical programs for quality and alignment of incentives. Advanced APM practices must have the infrastructure to support EHR use and share financial risks with the program; these practices can receive lump-sum bonus payments.
Pharmacists are currently not eligible to be MIPS providers. However, pharmacists’ activities can naturally affect the goals of the QPP through their daily clinical responsibilities, such as anticoagulation management, medication reconciliation and adherence, data collection, and care coordination. Practices should evaluate their operating models based on pharmacist-provided care models and, if they have not already, engage with pharmacists as effective, accountable care providers.
Medicare’s OCM and ASCO’s Patient-Centered Oncology Payment Model
The OCM refers to a CMS 5-year pilot program started in 2016 across 190 practices in 31 states with multiple commercial payers. The OCM aims to decrease cost, improve quality, and lower Medicare spending. OCM practices enter into contractual agreements requiring improved clinical standards, reporting of quality care metrics, and planning of data registries with quarterly submissions.
The OCM enhances the quality of the health system, with the value-based payment model that motivates patient-centered care and initiatives that drive outcome improvements. The pilot sets episode-based pricing and reimburses practices a Monthly Enhanced Oncology Services payment at the start of chemotherapy treatment of $160 per 6-month episode of care per patient, in addition to the regular fee-for-service per patient.20
The OCM aims to reduce unnecessary costs and variations in care through clinical oncology pathways, care coordination, and analysis of disease-specific variation. The OCM pilot and resulting data compared the performance among peer physician practices, highlighted patient-level data, and provided clinicians and administrators an in-depth understanding of their institutional needs for specific quality intervention. Key to influencing hospital administrators and to obtaining funding for new initiatives are data that can evaluate outcomes and analyze quality improvement processes and their impact on costs.
Alternative models have been proposed, such as the American Society of Clinical Oncology (ASCO) Patient-Centered Oncology Payment (PCOP) model, that match the workflow of patient treatment. Essentially, the model provides upfront money at the initial phase that includes diagnosis, choice of therapy, and counseling, and then provides monthly bundled payments during active treatment and management phases through 6 months after the last chemotherapy dose and during the monitoring and support phases. ASCO’s PCOP incentivizes providers to practice high-quality patient care, apply evidence-based use of clinical oncology pathways for drugs and tests, and adhere to ASCO standards of quality.
Another alternative model, MASON (Making Accountable Sustainable Oncology Networks) was approved in 2018 and defines oncology payment categories from a combination of clinical and claims data. Practices contribute 4% of fee-for-service money into a quality funds pool, which will be disbursed back to practices contingent on adherence to triage pathways, or referral processes for patients requiring urgent care, clinical pathways, or appropriate chemotherapy utilization across the continuum of care, as well as patient satisfaction with treatment.
Physicians expressed that, ideally, practices should receive new and continuous money across the patient treatment timeline so they could invest in practice redesign and value-based activities or transform into advanced APMs. Instead of including drug costs in the model, drug utilization and adherence could count as quality metrics that will affect shared savings. A fair model should incentivize the use of the right therapy for the right patient at the right time, with no concerns for cost, and must be dependent on value-based pathways, agnostic of the payer.
Value-Based Frameworks in Oncology
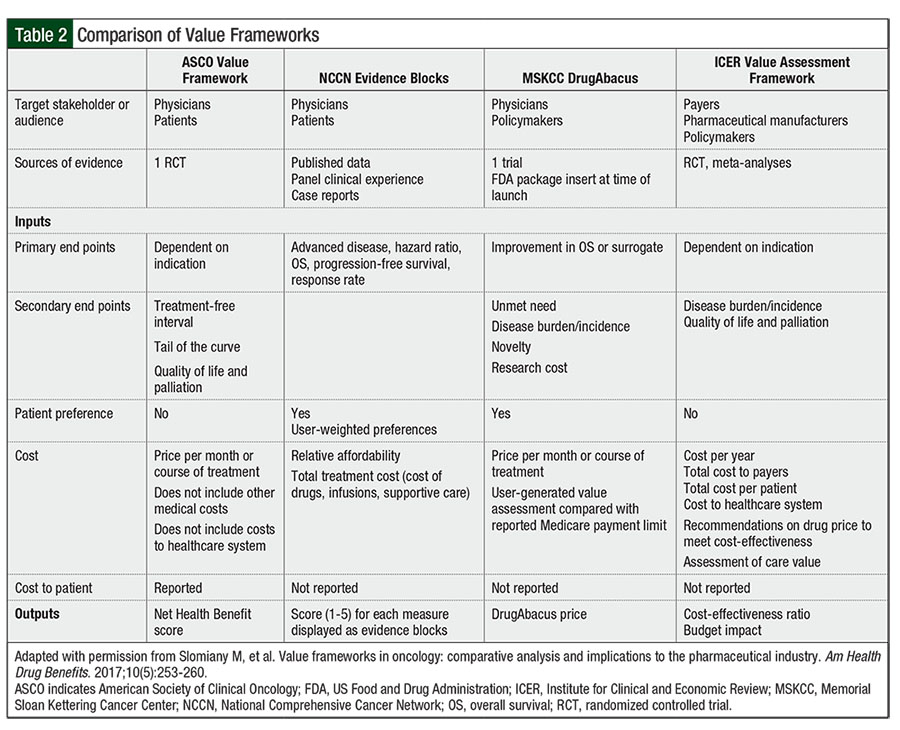
Value-based frameworks are intended as a tool to assess the value of a treatment and enable shared decision-making between patients and providers based on the clinical benefit, toxicities, and overall value to the patient. Value-based frameworks must adopt a patient-centered perspective and incorporate determinants of value and outcomes that are relevant to patients, such as additional years of life, years lived free of disease, functionality, independence, and absence of side effects.21,22
Value-based frameworks evaluate cost and use of therapies in a variety of disease states and are targeted toward different stakeholder perspectives across payers, providers, health systems, and patients.
Outcomes of a treatment may be measured across different dimensions of value, such as time to and sustainability of recovery, patient state of health, freedom from disease, nature of recurrences, and the need for intervention. Furthermore, measuring the results of implemented interventions will guarantee process improvement within healthcare organizations and result in continuous innovation in healthcare delivery.21,22 Value-based frameworks examine the value of a treatment looking at the larger population health data, to analyze overall costs relative to value added, including patients’ QOL during and after treatment, as well as societal costs.
Physician surveys reveal substantial variability in their understanding of value and awareness of value measurement tools. Surveys show that physicians and payers are split relative to the role of frameworks and their application in clinical practice. Lack of confidence in outputs limits a tool’s ability to inform decision-making for individual patients.23
ASCO, the Institute for Clinical and Economic Review (ICER), Memorial Sloan Kettering Cancer Center DrugAbacus, and the National Comprehensive Cancer Network (NCCN) have developed value-based frameworks to assist physicians, payers, and multiple stakeholders in their definition of value and in formulary management decision-making.23 Table 2 provides an overview and comparison of the 4 value-based frameworks discussed.23
At the forum, participants reviewed the 4 value-based frameworks from ASCO, ICER, NCCN, and the DrugAbacus for the measurement of treatment value and discussed their application in practice, strengths and weaknesses, and opportunities for pharmacists to shape better models in the future. Value tools increase awareness about overall costs and benefits of drug treatments to health systems and society, identify gaps in research, and empower patients and physicians. By providing a threshold or benchmark price relative to value, value-based frameworks can influence drug pricing, improve access to high-value treatment, advance patient-centered care, and enable robust decision-making.23
As value-based frameworks continue to evolve, opportunities exist in the use of real-world evidence to identify subpopulations that may benefit from treatment, as well as to introduce new efficacy and outcome measures in future clinical trials. In addition, critical to the optimization of value-based tools will be incorporation of the total costs of care in cost-effectiveness and price analyses and alignment of the incentives of all stakeholders for a potential consolidation of value-based assessments.
Collaboration across multiple stakeholders will be necessary to increase the adoption of value-based frameworks within health systems, achieve drug pricing aligned with a treatment value, and improve access to high-priced treatments. Increased involvement of pharmacists, patients, patient advocacy organizations, industry, employers, technology vendors, nurses, social workers, and other stakeholders will be critical to meet established quality measures.
Quality Measures in Oncology
The attainment of quality metrics ensures high-quality cancer care and motivates behavioral and practice changes within the oncology community.
The IOM defines healthcare quality within 6 domains—safe (avoiding harm), effective (treatments with proved benefit), patient-centered (respectful of patient preferences), timely (reduces wait for patients and providers), efficient (avoids waste of time, equipment), and equitable (equal irrespective of gender, ethnicity, social status) care.24
Performance measures by the National Quality Forum are defined across quality metrics, resource use and cost, value, and efficiency. Quality is measured across structures and processes of care (ie, appropriate diagnoses and tests) and overall outcomes of care. Intermediate and long-term healthcare outcomes include overall survival and reduced complications, and PROs include patient satisfaction with care and enhanced QOL.25
In addition, ASCO’s and other organizations’ contributions to the Choosing Wisely campaign highlight metrics that can lead to increased costs, such as inappropriate use of medical services and tests, lack of adherence to evidence-based guidelines, and other variations in care, all of which highlight the need to standardize cancer care.20
Oncology-specific quality measures were discussed at the forum and included those endorsed and published by national quality organizations and medical societies. Also discussed was the potential adoption of these measures in practice, and how they affect value. Oncology-specific MIPS quality measures increasingly focus on patient-reported experience and satisfaction in care, processes to ensure that chemotherapy-related complications are managed in a timely fashion, clinical interventions for pain, advance planning for end-of-life care, and patient outcomes. Forum participants discussed imminent MIPS measures on the horizon, such as chemotherapy in the last 14 days of life, hospice length of stay within 30 days of death, and cancer-specific mortality rate.
The Quality Oncology Practice Initiative (QOPI) certification, a quality program endorsed by ASCO, is issued to practices that perform at the highest levels of competence in patient care delivery. This program counts as a MIPS quality improvement measure. QOPI standards consist of creating an environment that ensures excellent patient care and safety. Clinical performance is measured across processes of care delivery encompassing general policy; chemotherapy handling and administration; adherence to treatment; follow-up on toxicity and complications; treatment planning, staffing, and patient education.
Barriers to adoption of quality metrics in oncology were identified. The burden of data collection leads to lack of visibility of key clinical and social data that may affect performance scores. The cost of cancer care is subject to considerable variability of cancer subtypes, mutations, patient comorbidities, treatment history, and financial toxicity—all necessitating reliable population health data to inform value-based programs.
Social determinants of health, such as a patient’s socioeconomic status, health literacy, food security, and access to transportation, affect treatment outcomes and must be adjusted for in quality measurements. For example, patients with low socioeconomic status have reduced ability to engage in self-care and prevention of side effects, and a higher risk for hospitalizations and healthcare utilization.
Similarly, cancer stage information and risk levels are missing from Medicare claims data, leading to unstable bundles with high variability in patient risk levels. Essential diagnostics data to inform physicians are scattered in patient charts, locked in PDF documents within the EHR system, and are not disseminated between care centers such as urgent care, clinics, infusion centers, and palliative centers.
Learning health systems that can quickly analyze data are urgently needed to answer clinical questions, modify toxic chemotherapy regimens, and be useful in point-of-care clinical decision-making. Vendors must be involved in discussion of value measurements and should direct their efforts toward designing enhanced, user-friendly EHR technology, to facilitate meaningful accessibility and real-time data sharing across healthcare providers, institutions, and payers.
Discussion
Ample opportunities exist for pharmacists within the multidisciplinary care team to fully engage with physicians, patients, and payers to ensure the delivery of high-value oncology care. Clinical and health system pharmacists must be involved in direct patient care, empower physicians in the use of clinical pathways, assist in end-of-life care, suggest clinical study design, and enroll patients in clinical trials. Increased pharmacist involvement in clinic activities, such as assessing laboratory tests, ordering tests, and managing patients, increases efficiency and helps to manage patient volume.
The HOPA/AMCP forum panel members representing health systems discussed examples of successful collaboration between health systems and payers enabling data exchange and risk stratification of patients, and subsequent reorganization of pharmacy resources from volume to value-based activities. They described how pharmacist teams within their organizations are significantly contributing to chemotherapy pathways tailored to patient characteristics and working on categorization of cost-effective regimens into appropriate patient bundles.
Critical to cementing the role of pharmacists as providers of value within their institutions is the ability to measure outcomes of value-based activities by evaluating changes in adherence rates, number of emergency department visits and readmissions, and overall cost-savings. Armed with these data, pharmacists can demonstrate their own value and approach their respective organizations with proposals of cost-effective, practical processes and additions of infrastructure that can support pharmacy-specific initiatives in the delivery of high-value cancer care.
Conclusion
The shift to value-based reimbursement has transformed the delivery of oncology care within hospitals and physician practices. Strong collaborations among stakeholders within the healthcare system, such as hospitals, public and private payers, professional organizations, and data analytics, will be necessary to reach consensus on value frameworks, standardize delivery of care across populations, and complete real-time data analytics to build a model of precision delivery to every patient. The 2019 HOPA/AMCP forum provided a venue to discuss the value-based care model. The role of the pharmacist within this model has not been defined. As pharmacy leaders, we must start the conversation within our practices that will further shape our roles and address many unanswered questions.
This forum discussion serves as a call to action to health system pharmacists to engage in the continuum of cancer care as an essential provider of value through the implementation of quality processes that inform safe and effective treatment choices, enhance patient satisfaction with care, and reduce unnecessary healthcare costs. Participants proposed value-based interventions and discussed barriers to the delivery of cost-effective oncology care.
At the forum, representatives of the HOPA and AMCP organizations affirmed their shared commitment to advancing patient care and improving clinical outcomes in oncology. Recommendations gathered at the forum for pharmacists to engage in the practice of value-based oncology care will be shared with patient groups, providers, and policymakers and will be used to move this conversation forward.
References
- Institute of Medicine. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC: National Academies Press; 2013.
- Tran G, Zafar SY. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6:166.
- Centers for Medicare & Medicaid Services. 2019 Merit-based Incentive Payment System (MIPS) Quality performance category fact sheet for individual MIPS eligible clinicians, groups, and virtual groups. Updated January 2020. https://qpp.cms.gov/mips/quality-measures. Accessed July 21, 2020.
- Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318:197-198.
- Polite B, Walradt J. Pursuing value in cancer care: a model in progress. J Oncol Pract. 2017;13:407-409.
- Panattoni L, Fedorenko C, Greenwood-Hickman MA, et al. Characterizing potentially preventable cancer- and chronic disease–related emergency department use in the year after treatment initiation: a regional study. J Oncol Pract. 2018;14:e176-e185.
- Hunis B, Alencar AJ, Castrellon AB, et al. Making steps to decrease emergency room visits in patients with cancer: our experience after participating in the ASCO Quality Training Program. J Clin Oncol. 2016;34(7_suppl):Abstract 51.
- Nigro SC, Garwood CL, Berlie H, et al. Clinical pharmacists as key members of the patient-cN network of the American College of Clinical Pharmacy. Pharmacotherapy. 2014;34:96-108.
- Joseph T, Hale GM, Eltaki SM, et al. Integration strategies of pharmacists in primary care-based Accountable Care Organizations: a report from the Accountable Care Organization Research Network, Services, and Education. J Manag Care Spec Pharm. 2017;23:541-548.
- Clifton CL, Branham AR, Hayes HJ, et al. Financial impact of patients enrolled in a medication adherence program at an independent community pharmacy. J Am Pharm Assoc. 2018;58:S109-S113.
- Matzke GR, Moczygemba LR, Williams KJ, et al. Impact of a pharmacist–physician collaborative care model on patient outcomes and health services utilization. Am J Health Syst Pharm. 2018;75:1039-1047.
- Leary MH, Morbitzer K, Walston BJ, et al. Evaluation of targeted pharmacist interventions to reduce length of stay in an acute care practice model. Ann Pharmacother. 2019;53:471-477.
- Cothran T, Holderread B, Abbott M, et al. The pharmacist’s role in shaping the future of value-based payment models in state Medicaid programs. J Am Pharm Assoc (2003). 2019;59:121-124.
- Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34:557-565. Errata in: J Clin Oncol. 2016;34:2198; J Clin Oncol. 2019;37:528.
- Dieguez G, Ferro C, Pyenson BS. A multi-year look at the cost burden of cancer care. Milliman; April 11, 2017.
- Gidwani-Marszowski R, Nevedal AL, Blayney DW, et al. Oncologists’ views on using value to guide cancer treatment decisions. Value Health. 2018;21:931-937.
- Kreys ED, Koeller JM. Documenting the benefits and cost savings of a large multistate cancer pathway program from a payer’s perspective. J Oncol Pract. 2013;9:e241-e247.
- Lipitz-Snyderman A, Sima CS, Atoria CL, et al. Physician-driven variation in nonrecommended services among older adults diagnosed with cancer. JAMA Intern Med. 2016;176:1541-1548.
- Institute of Medicine. The Learning Healthcare System: IOM Roundtable on Evidence-Based Medicine. Washington, DC: National Academies Press; 2007.
- Polite BN. Achieving value in oncology: a 5000 to 50 foot view. The University of Chicago Medicine: The OCM Journey. https://unclineberger.org/outcomes/files/2018/09/20180213-breakfast-seminar-polite.pdf. Accessed July 21, 2020.
- Waldeck AR, Botteman MF, White RE, van Hout BA. The importance of economic perspective and quantitative approaches in oncology value frameworks of drug selection and shared decision making. J Manag Care Spec Pharm. 2017;23(6-a suppl):S6-S12.
- Porter ME. What is value in health care? N Engl J Med. 2010;363:2477-2481.
- Slomiany M, Madhavan P, Kuehn M, Richardson S. Value frameworks in oncology: comparative analysis and implications to the pharmaceutical industry. Am Health Drug Benefits. 2017;10(5):253-260.
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- National Quality Forum. Patient-reported outcomes. www.qualityforum.org/Patient-Reported_Outcomes.aspx. Accessed January 20, 2020.
View Publication